Pelvic Organ Prolapse: From Symptoms to Solutions

What is Pelvic Organ Prolapse?
Pelvic organ prolapse (POP) is a disorder in which the muscles and tissues of the pelvic floor can no longer adequately support the pelvic organs and they drop down or press into the walls of the vaginal canal. Three different types of POP are illustrated below. These are named based on the pelvic organ that is descending.
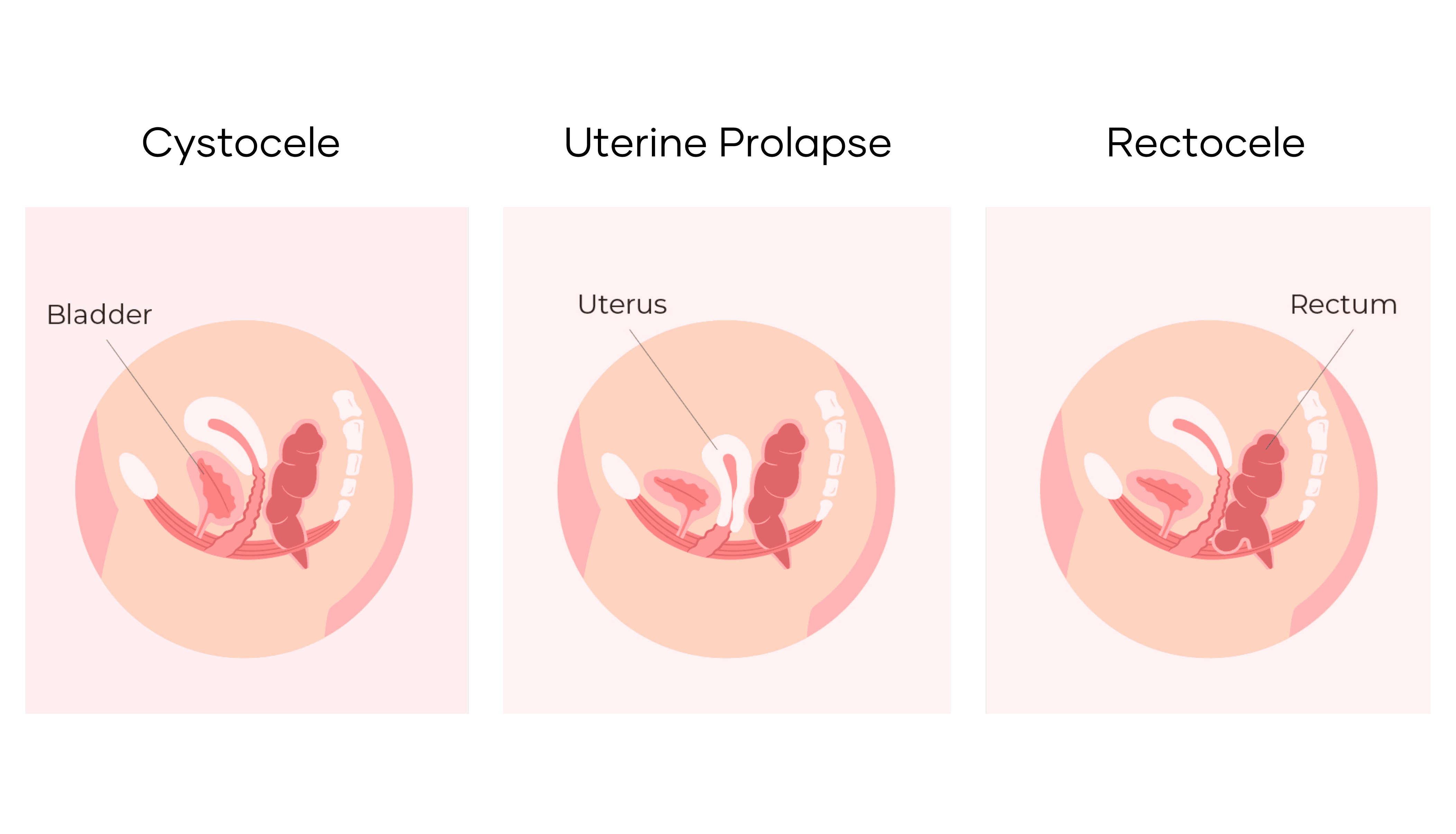 A cystocele occurs when the bladder drops into the vaginal canal, a uterine prolapse occurs when the uterus drops into the vagina, and a rectocele occurs when the rectum bulges into the vagina.
A cystocele occurs when the bladder drops into the vaginal canal, a uterine prolapse occurs when the uterus drops into the vagina, and a rectocele occurs when the rectum bulges into the vagina.
POP prevalence increases as a woman ages. In fact, 74% of women between 40-59 have POP. However, aging is not the only risk factor for this condition. Other common risk factors include genetics, connective tissue disorders, obesity, pelvic floor injuries, hysterectomies, and hormonal changes associated with menopause and pregnancy. POP can also occur following childbirth and is particularly seen in women who’ve had multiple vaginal deliveries and/or given birth to a baby weighing more than 8.5 lbs.
Additionally, habits or activities that cause excessive strain on the pelvic floor can also lead to POP. Examples include constipation, chronic coughing due to smoking or lung disease, and high-impact exercise or jobs that require heavy lifting. The symptoms impact physical as well as mental health.
Symptoms
The symptoms of POP can be very debilitating for some people, however, not all individuals who have POP will experience symptoms. In rare circumstances, POP can occur suddenly as a result of significant strain causing the last bit of connective tissue that is supporting the pelvic organ to give way. However in most cases, women begin experiencing a variety of pelvic symptoms that worsen over a period of time, until the actual prolapse is discovered.
Symptoms of POP can include:
- Sensation of vaginal bulging or heaviness, like “something is falling out”
- Pelvic pressure, dullness, aching or discomfort that progressively worsens as the day goes on, or with activities that can cause downward strain such as high-impact exercise and/or coughing
- Urinary leakage or inability to fully empty bladder
- Difficulty having bowel movements and fully emptying stool
- Difficulty inserting tampon
- Painful intercourse
- Low back pain
Diagnosis
POP is diagnosed via a pelvic examination performed by an OB/GYN or urogynecologist. To assess the severity of the prolapse, individuals are asked to cough or bear down, which replicates the effect of increased intraabdominal pressure on the pelvic organs. The provider will then grade the severity of the prolapse based on how far the organ drops in relation to the vaginal opening. If the prolapsing portion does not drop past the vaginal opening, the prolapse is considered grade 0-2. If the prolapsing portion drops partially (3) or completely (4) past the vaginal opening, it is considered grade 3-4.
In some cases, it can be difficult to accurately identify which organ is prolapsed. Therefore, some providers will classify the type of POP by the part of the vagina that is prolapsing (front, top, back) and not the actual pelvic organ.
Impact on Quality of Life
The severity in which POP impacts one’s quality of life (QOL) varies widely. For some women, POP can be a minor frustration that can be managed by avoiding certain activities that may cause symptoms. For those with severe symptoms, POP can greatly impact all areas of their life, including their mental health.
Below are some examples of how POP can impact QOL:
- Negative beliefs about themselves and their bodies
- Pain with intimacy or fear of intimacy
- Avoidance of high impact exercise (ex: heavy weight lifting, jumping, running)
- Physical difficulties with symptom aggravation by occupational duties
Care Options
There are a variety of different treatment options for POP including surgery, pessary usage, obesity management, and pelvic-floor therapy.
1. Surgical Intervention Surgical intervention can include using body tissue or synthetic mesh to repair the prolapse and provide pelvic support for the organs. Research indicates that by age 79, women have an 11% chance of undergoing at least one surgery for POP or incontinence, with this risk potentially doubling in the next 30 years due to an aging population. Unfortunately, the long-term outcomes of POP surgery are not favorable. After 5 years, 41% of women who underwent surgery for POP experience recurrence and 10% required another surgery.
2. Pessary Usage A pessary is a removable device that is inserted into the vagina to provide support to the vaginal walls and pelvic organs. Pessaries are a non-invasive treatment option that may help reduce the symptoms of POP and urinary incontinence. They are often used in conjunction with other treatment options including weight management and pelvic floor strengthening to maximize symptom relief.
3. Obesity Management and Diet Since excess weight within the abdomen causes added pressure on pelvic organs and the pelvic floor, maintaining a healthy weight may prevent POP from occurring. For individuals with POP who are overweight, weight loss is a recommended treatment option. Typically this involves a combination of exercise and dieting. Individuals are also encouraged to eat a high-fiber diet to prevent constipation and the need to strain with bowel movements.
4. Pelvic-Floor Therapy Pelvic therapy is another non-invasive option to address the symptoms of POP. Pelvic therapy can not only reduce the severity of symptoms in those already suffering from POP, but also may help decrease the development of POP. Pelvic-floor therapy often includes a combination of the following:
- Exercises to strengthen the pelvic and abdominal muscles for increased support of pelvic organs.
- Activity modification to reduce the amount of pressure placed on pelvic organs.
- Bladder/bowel training to promote healthy habits around toileting.
How Bloom Can Help
Bloom offers digital pelvic-health care for individuals suffering from POP. With Bloom, individuals are paired with a Pelvic Health Specialist that has a Doctor of Physical Therapy degree to help address the symptoms using a variety of techniques including strengthening exercises, activity modifications, and bladder/bowel training.
Bloom helps individuals improve their pelvic-floor and abdominal muscles through a customized exercise program, guided by their Pelvic Health Specialist. During the exercise sessions, members use the Bloom Pod by Elvie—Bloom’s FDA-listed device offers real-time feedback by aiding members in correctly performing the pelvic therapy exercise sessions. Upon completion of a session, members can instantly view their results and track their progress throughout their journey to better pelvic health.
The Sword Health App also provides access to Academy, which includes a library of videos from clinical experts to help members better understand their pelvic health, reduce risks, and build healthy habits. These videos provide actionable tips for managing POP, including behavioral strategies such as core pressure management, and ways to quickly manage and relieve uncomfortable pressure on the pelvic floor. Academy also provides education on how to optimize bladder and bowel health with instruction on digestive massage techniques, dietary considerations, and healthy bladder and bowel habits, to prevent recurrence of prolapse in the future.
Additionally, if surgery is part of the overall treatment plan, Bloom may even help augment surgical outcomes, pre- and post-operatively.
Bloom is available through employers and health plans. Learn more about Bloom.
While we use the word "women" in some of our communications, Bloom is designed for all individuals with vaginal anatomy regardless of gender identity.
DISCLAIMER
This article is intended for educational purposes only, using publicly available information. It is not medical advice nor should it be used for the diagnosis, treatment, or prevention of disease. Please seek the advice of your physician or another licensed medical provider for any health questions or concerns. In case of emergency, call 911.


